All over the world, many researchers are working tremendously hard to create a brighter future for children with cancer. In the UK and Ireland, over 100 of these researchers have been funded through CCLG.
We fund our own research, and we also support other charities to fund research through the CCLG Charity Research Funding Network. Our goal is to enable childhood cancer charities to fund the research that is important to them, but with the support of our rigorous and accredited research process and our specialist expertise. This makes sure that funding is used for high quality research that is likely to have a real impact.
But what does this impact look like? Let’s take a trip to the University of Oxford to find out about three of the projects we have been involved in funding there…
How do leukaemia stem cells talk to the immune system in juvenile myelomonocytic leukaemia? with Professor Adam Mead
Around ten children are diagnosed with juvenile myelomonocytic leukaemia (JMML) each year in the UK, making it one of the rarer types of leukaemia that children can get. Unlike some of the more common types of leukaemia, JMML is hard to treat. The only known effective treatment is a stem cell transplant, and this is not always successful.

Professor Adam Mead
Adam’s project was funded last year by CCLG Special Named Funds. In the project, he hopes to understand why JMML can come back after a stem cell transplant so that he can find a way to prevent it.
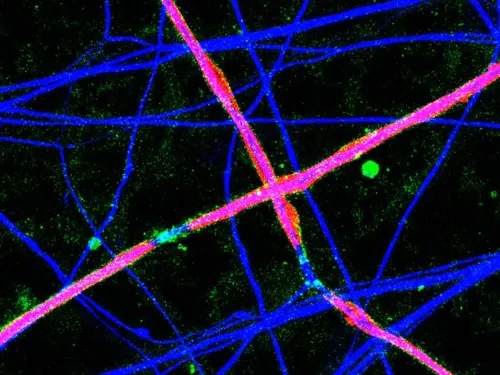
Adam is focusing on a type of cell called a JMML leukaemia stem cell. These cells can avoid being killed and are the reason the cancer comes back after stem cell transplants. Adam’s previous research suggests that the leukaemia stem cells turn off the immune system, so it can’t fight off any leukaemia cells that have survived the transplant.
If his team can find out how the leukaemia stem cells talk to the immune system, they might be able to develop treatments that block this communication. This would allow the immune system to kill off all the leukaemia cells.
He said: “The purpose of this project is to study the JMML leukaemia stem cells at different timepoints in the patient journey.
“With our previous work in JMML we were able to identify JMML stem cells, which are the cells that give rise to the leukaemia, and through this project we will study which of the cells’ vulnerabilities could be utilised for the design of novel and more effective therapies.
Our ultimate goal is to enable scientists to design new treatments for JMML and to directly improve the prognosis of this aggressive leukaemia.
Understanding a potentially new therapeutic target in incurable childhood acute lymphoblastic leukaemia with Professor Anindita Roy
Anindita is also working on leukaemia but is focusing on the most common type in children – acute lymphoblastic leukaemia.
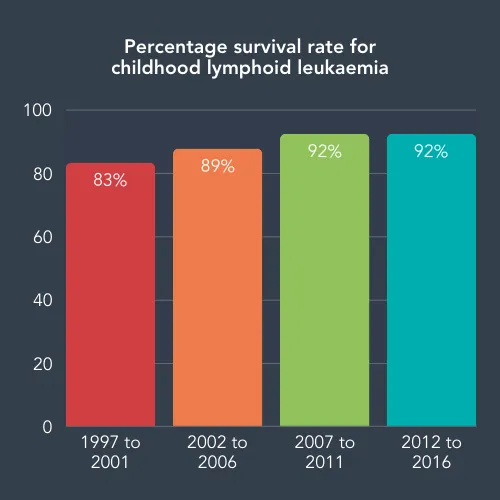
Acute lymphoblastic leukaemia is the success story of childhood cancer, going from under 10% of children surviving their diagnosis in the late sixties to a current survival rate of over 90%. This was achieved through years of research to find which patients were at risk of the cancer coming back and for new combination treatments.
However, the fantastic 90% overall survival rate is not the same for across different ages. Only half of children diagnosed with leukaemia before their first birthday survive, and researchers don’t fully understand why. However, we do know that these patients often have a type of leukaemia that has errors in the MLL gene. This gene usually regulates other genes that control cell growth, replication, and death. The MLL errors can help the leukaemia grow and replicate faster, and so is a key research focus.

Professor Anindita Roy
By creating a model of MLL leukaemia in the lab that behaves like real patients’ cancer, Anindita has shown that this type of leukaemia often needs a protein called CD133 to survive. Funded by the Little Princess Trust, her project looks to understand how this protein helps leukaemia cells survive treatment.
To understand CD133 fully, she wants to find out whether MLL leukaemia can survive and grow without it, and compare how the protein is regulated in healthy cells and in MLL leukaemia cells.
Over the past two years, she has discovered that leukaemia cells which contain lots of CD133 grow faster and more aggressively than those without. When there is less CD133, the leukaemia cells grow much more slowly.
Anindita hopes that her findings will lead to new treatments, such as immunotherapies that target treatment-resistant cancer cells by looking for CD133 proteins.
Understanding why some childhood blood cancers are incurable with Professor Anindita Roy
Anindita is also taking the above methods and applying them to other types of acute lymphoblastic leukaemia to find out what the cancer cells depend on and how they develop. Her project on understanding why some childhood blood cancers are incurable is funded by our fantastic Special Named Fund families and started in August last year.
Despite the amazing improvements in leukaemia survival rates over the past five decades, they have not improved significantly within the past few years. We need to understand more about acute lymphoblastic leukaemia, such as why it can come back after treatment and what gene mutations make it harder to cure.
The model of MLL leukaemia Anindita created in her other project was a major breakthrough for infant leukaemia research. Anindita is now developing similar models for other high-risk childhood leukaemias in this project. These models, alongside cells from patients, will allow her to look at which genes are not behaving as expected, and how these errors affect how the cancer cells grow and spread.
Her team already has collaborations planned, so any findings from this project can quickly be translated into new immunotherapy treatments. Anindita hopes that her work will lead to improvements in the survival rate for children with high-risk leukaemia.
She said:
As a clinician myself, I never lose sight of why we are doing the research - always for the benefit of the children affected by leukaemia. We hope that our efforts will eventually lead to a meaningful improvement in survival and quality of life for children with high-risk leukaemia.

Ellie Ellicott is CCLG’s Research Communication Executive.
She is using her lifelong fascination with science to share the world of childhood cancer research with CCLG’s fantastic supporters. You can find Ellie on X: @EllieW_CCLG