When your child has symptoms that could be caused by cancer, they will be referred by their GP or local hospital to one of the following specialists:
- a paediatrician, who specialises in treating children
- a paediatric oncologist, who specialises in treating children with cancer
- a paediatric haematologist, who specialises in treating blood disorders
Most children with cancer will be treated in a Principal Treatment Centre within a hospital. Teenagers may be treated in a unit specially designed for teenagers and young adults with cancer.
When Jonathan was diagnosed with leukaemia, it was a massive shock to us. What a world away from playing with his little brother on a hot sunny day just 24 hours earlier!Marie, mum of Jonathan diagnosed with ALL
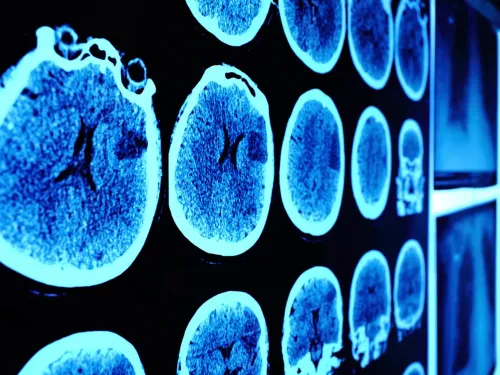
Tests and scans
Various tests and scans will be done to diagnose your child's illness and to monitor your child throughout treatment.

Staging
The stage of a cancer means the size of the tumour and whether or not it has spread beyond where it started in the body. Knowing the extent of the cancer helps doctors decide on the best treatment for your child.
Advice from our experts
"When your consultant gives you the news of your child's diagnosis they should explain what this means and what treatment is recommended. Sometimes this happens straightaway, at other times the results of further tests may need to be available before the final recommendations for treatment can be made.
It is difficult to remember everything from those meetings as there is so much information and you may find it hard to concentrate in what can be a very stressful situation. You should have a key worker who is usually a specialist nurse. If she or he can sit in on the conversation with the consultant they can go over things again with you later.
Ideally, your consultant should copy you into the correspondence to your GP or write specifically to you summarising your conversation. If you still have questions, you should ask for another meeting with your consultant to go through those.
Questions you might want to make sure have been answered are:
- What is the exact diagnosis?
- Has the disease spread anywhere else?
- What is the proposed treatment?
- How long will it take?
- Where will it take place?
- When can my son/daughter go back to nursery/school?
- Are there any other treatments available?
- Are there any clinical trials of treatment available in our centre or elsewhere?
- How successful is treatment likely to be?"
Dr Martin English
Consultant Paediatric Oncologist, Birmingham Children's Hospital, UK
CCLG member and previous Contact magazine's Medical Adviser
"Your child's diagnosis should be discussed at the multi-disciplinary (MDT) meeting in the main hospital where you are diagnosed. In most cases, there will be other consultants on the team as well and you could ask to see one of them as well.
If you would like your child's case discussed in another hospital, you should ask your consultant to refer you for a second opinion to another principal treatment centre. Most consultants in other hospitals will want to review your child's scans and sometimes the biopsies themselves in their own MDT meeting before seeing you for a second opinion themselves. These would be referrals within the NHS and should not incur any charges for you.
Sometimes families want to seek second opinions from teams in other countries. It is more likely that your consultant will ask you to make those contacts yourself, but you can ask for a summary of your child's case and ask for copies of scans. The hospital may charge you for the cost of scans copied for yourself. You may find that some hospitals abroad make charges for opinions and for treatment.
Your consultant themselves may ask the MDT in another main hospital or sometimes colleagues abroad for their opinion in some cases. They should, of course, ask your permission to do this, but there would be no costs to you for this."
Dr Martin English
Consultant Paediatric Oncologist, Birmingham Children's Hospital, UK
CCLG member and previous Contact magazine's Medical Adviser
"There are a small number of very rare genetic syndromes that are associated with increased risk of developing childhood cancer. However, these account for fewer than 1 in 20 of all new childhood cancers diagnosed. For most children the cause is not clear and it is extremely rare for more than one child to be diagnosed within the same family."
Dr Richard McNally
Research Academic, Royal Victoria Infirmary, Newcastle Upon Tyne, UK
CCLG member and Chair of CCLG's Epidemiology Group
"Some chemotherapy drugs can be irritant to the veins and if they are given through an ordinary drip in to the veins in the hands and arms these quite quickly become scarred and it can be difficult to get drips in which can be painful and distressing.
Also some of the drugs that are given can cause chemical burns to the tissues and skin if they leak in to the tissues from the veins. It is likely that blood samples may need to be drawn, and antibiotics and blood transfusions given in between chemotherapy treatments and it is much less distressing for your child if these can be given through a central line or portacath."
Dr Martin English
Consultant Paediatric Oncologist, Birmingham Children's Hospital
CCLG member and previous Contact magazine's Medical Adviser
"There is some limited evidence to suggest an association between exposure to high strength magnetic fields and increased risk of childhood leukaemia. However, very few homes in the UK are exposed to these sorts of levels of magnetic fields from power lines. So, it is very unlikely that the possible exposures from the nearby power lines would have caused the child's cancer."
Dr Richard McNally
Research Academic, Royal Victoria Infirmary, Newcastle Upon Tyne, UK
CCLG member and Chair of CCLG's Epidemiology Group

