Have you ever started a project with a clear goal in mind, only to end up somewhere completely different? Maybe you picked up your phone to check one email and suddenly realised you were still scrolling two hours later, or began a ‘quick tidy’, only to end up reorganising the whole house at 2 am.
Science can be a lot like that - especially when developing medicines. It can be almost impossible to identify all the ways a medicine will interact with our bodies. This means that, sometimes, medicines have effects that aren’t part of the disease they’re intended to treat – like blood pressure medicine helping with migraines.
‘Repurposing’ takes advantage of this by using existing, approved drugs to help treat other diseases – such as looking at whether diabetes medicines can treat cancer. It sounds surprising, but this approach is already helping researchers find new uses for old drugs. Developing an entirely new drug can take over a decade and cost over a billion pounds. Using medicines that are already known to be safe for humans saves time and money, meaning that patients see new treatments sooner.
How could repurposing help children with leukaemia?
Dr Nick Jones is a researcher at Swansea University working on repurposing drugs for T-cell acute lymphoblastic leukaemia (T-ALL) – an aggressive and hard to treat type of childhood leukaemia. Around one in five children with T-ALL will have their cancer become resistant to treatment or grow back afterwards, which makes further treatment much harder.
Nick said:
We've taken massive strides since the 1960s in treating T-ALL in children. But there is still an unmet clinical need for those children who relapse, which is our main focus. However, even for good outcomes, the type of treatment that the children receive has long lasting side effects in some cases.

Dr Nick Jones
In 2021, funded by The Little Princess Trust, his team began investigating whether a diabetes medicine called canagliflozin could kill T-ALL cells.
“Canagliflozin was developed to block a protein that transports glucose into the cell,” said Nick. “However, it unintentionally also targets the proteins that are involved in cell metabolism.”
Because T-ALL cells are growing quickly and out of control, they need a lot of fuel to keep going. By targeting metabolic proteins, canagliflozin essentially blocks the cancer cells’ access to their favourite fuel sources – potentially offering a way of starving and killing the cancer.
A surprising setback
Nick’s team tested canagliflozin on cancer samples from children with T-ALL, cells grown in the lab, and mice with T-ALL. From previous investigations, they expected it to kill the T-ALL – but the adaptable cancer had other plans.
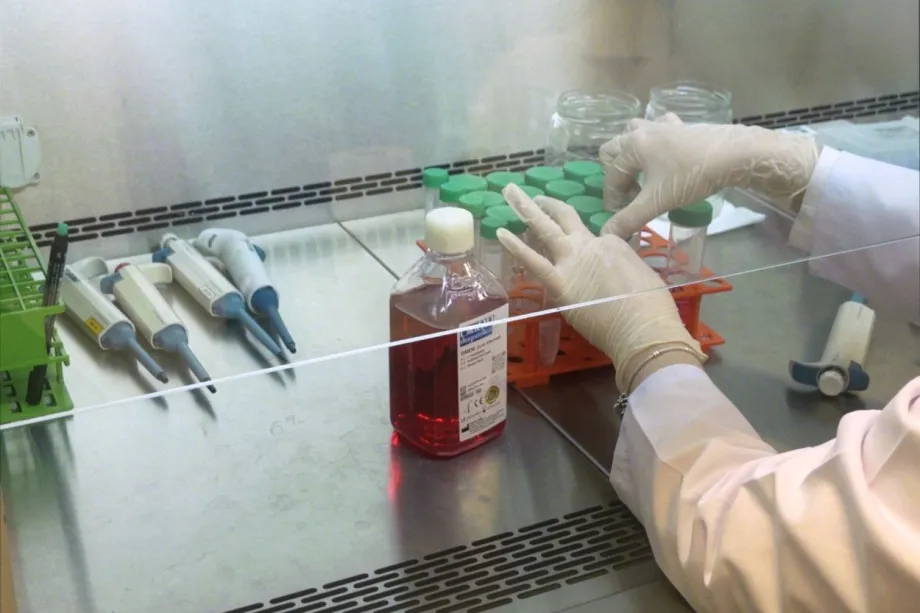
Growing leukaemia cells in the lab.
Instead of using its usual fuel sources, the cancer switched to different nutrients (serine and glycine), making it more resistant to canagliflozin. chemotherapies. This result was unexpected but beneficial as it flagged up a process that the cancer was using to survive which could potentially be targeted to stop the cancer from becoming resistant.
A new way forward
Nick’s team were keen to investigate further, so they developed models to see what happens when the cancer can’t access those backup fuel sources. In these models, canagliflozin was able to kill over 60% of T-ALL cells in the lab within three days. In other words, removing the key amino acids (serine and glycine) made the drug far more effective.
Nick suggests this provides evidence for a combination treatment that uses canagliflozin alongside a medically prescribed diet that limits the serine and glycine available for the cancer. However, he caveated that “any growing child will need nutrients to grow, so a lot of care has to be taken with this.”
The next stage for this research is to test the combination treatment even further in the lab to make sure that it is safe and effective for as many patients as possible. With more research, this approach could lead to safer and smarter options for those children with specific leukaemia types who desperately need new treatments.

Ellie Ellicott is CCLG’s Research Communication Executive.
She is using her lifelong fascination with science to share the world of childhood cancer research with CCLG’s fantastic supporters. You can find Ellie on X: @EllieW_CCLG




