When your child is diagnosed with cancer, there is a lot to understand on top of feeling anxious and worried about the future. The first mention of palliative care can sound scary as people can think that it means treatment has not worked, raising questions about whether your child will recover or not. However, palliative care is far more than just end-of-life care. So, what exactly is it?
Palliative care as supportive care
Palliative care is all about supporting the child, and their family, to live their best quality of life for as long as possible. Relieving symptoms is a key part of this, for example using anti-nausea medicines to help with chemotherapy-related sickness. Mental health is important too, so palliative care professionals might offer therapy to help children cope better with treatment, or counselling for parents. It can be given right from diagnosis, at any stage of the journey for all patients - including whilst having treatment to cure their cancer.
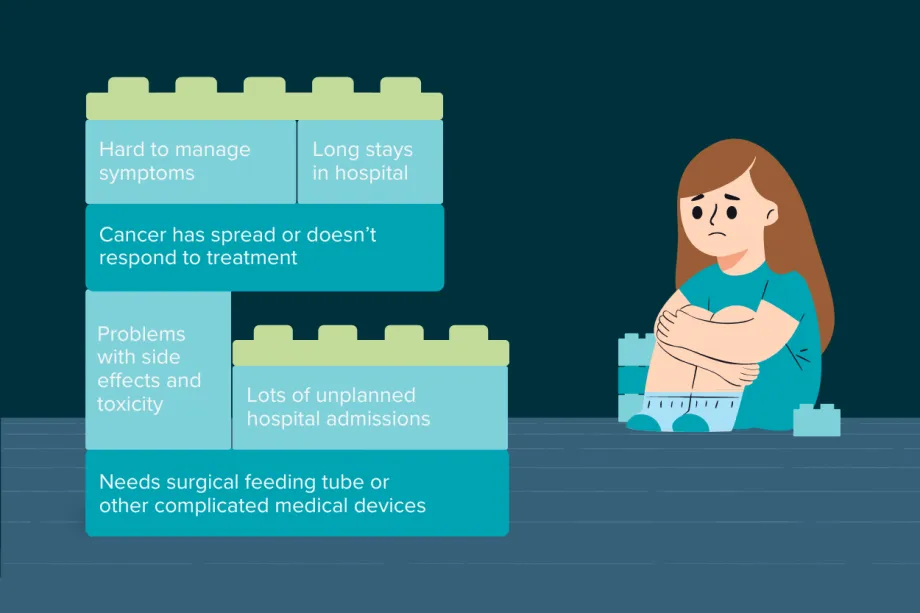
In addition to a cancer diagnosis, there are indicators that mean palliative care could be useful for a child.
Palliative care can also be called ‘supportive care’ and is an essential part of cancer care, covering anything that makes a child's cancer journey easier. Some hospitals use palliative care and supportive care interchangeably. At others, the term ‘palliative care’ is not widely used because families can think that it is for end-of-life care only. However, WHO guidance increasingly recommends that palliative care is a standard part of childhood cancer care because it can improve children’s quality of life.
Research at the MD Anderson Cancer Center in Texas found that doctors were less likely to refer patients to a palliative care service - even if it provided the same help as a supportive care service. Doctors felt that the words ‘palliative care’ were more distressing for patients and families. After renaming the service to 'supportive care', there were 41% more referrals. There was also evidence that suggested patients were being referred earlier in their cancer.
Whole family support
It’s not just about medicines and treatments – palliative care also covers the social and spiritual needs of the patient and family. Going through cancer, and watching your child go through cancer, takes a huge emotional and psychological toll. Parents might need help explaining concepts to their child, such as why they are ill, and may need support with their own mental health.
A child’s emotional distress about procedures or treatments can worsen their experience, for example, preventing pain management from working effectively. Similarly, if a family member is upset, it can impact the child. This makes caring for the whole family, with respect to their cultural and spiritual identity, a vital part of childhood cancer care.

There are lots of people who can help with palliative care. Children might have care from the palliative perspective with their main care team, or could be referred to a special service. Palliative care professionals care for every aspect of a young perso
Care teams might also discuss advanced care planning. This is a roadmap of what is important to a child and their family about their care. It plans how a child should be cared for in different circumstances, like in emergencies or if they can no longer be cured. It does not mean their cancer is incurable, but ensures that they are properly supported if their cancer progresses.
For example, this might mean the care team works hard to keep a child at home, where they feel safe. Advanced care plans are very personalised and can be updated to suit each child as they grow and their priorities change. Parents and their child, if age-appropriate, can work with the care team to create a plan. This empowers families to make informed decisions and ensures that care aligns with the child's values and wishes.
Hospice care
Hospices are experts at palliative care. They are not just for end-of-life care. Instead, they can provide support at home, take patients in for a day, for respite breaks, or on a longer-term basis. The common idea of hospices as depressing places couldn’t be further from the truth – have a look at Rainbows, a hospice in Leicestershire:
Children can be referred to a hospice at any stage of their cancer, much like palliative care. The hospice team will work hard to make sure the child has the best quality of life possible. Hospices might help children with complicated needs that can’t be managed alone at home. They can also take care of children for a little while to allow parents and carers to recharge or spend time with other children. Caring for a child with cancer takes a huge emotional and mental toll, so breaks can be really important to allow families to support their child in the long term.
End-of-life care
Sadly, not every child can be cured of their cancer. ‘End of life’ is the period leading up to death, a period that can be anywhere from days to months. The main objective is to keep the child comfortable. This means avoiding any unnecessary tests or procedures that wouldn’t improve their quality of life or survival. For example, chemotherapy that does not manage cancer symptoms could be stopped.
Children and families can usually, barring complicated medical needs, choose where to stay for this care. This might be at home, in a hospice, or in a hospital. Palliative care teams can help parents explain what is happening to their child, and help families decide what is important to them.

End-of-life care encompasses not only the physical, but also emotional and psychological support for the child and their family. For example, families could have access to counselling, support groups, and help coping with their grief and loss.
Changing views
The use of palliative care is increasingly recommended as a standard part of childhood cancer treatment. However, there is still a long way to go before palliative care becomes the norm. One study, focused mainly on high-income countries, found that only 55% of children with cancer were offered any specialised palliative care before passing away. It is vital that palliative care, or supportive care, is available for children with cancer and their families. It can make a huge difference in quality of life during and after treatment.
Palliative care treats patients as whole people. It cares for the emotional, social and spiritual issues, as well as the physical symptoms. Open and honest communication between families and professionals is key to palliative care and also not to be scared of the name – if you feel like you need extra help, please talk to your care team about what palliative or supportive care they could offer.

Ellie Ellicott is CCLG’s Research Communication Executive.
She is using her lifelong fascination with science to share the world of childhood cancer research with CCLG’s fantastic supporters. You can find Ellie on X: @EllieW_CCLG




